Why Should You Test for Epstein-Barr Virus?
Testing for Epstein-Barr Virus (EBV) is important for helping to identify viral triggers. Symptoms can be persistent and similar to many other viruses, which warrants investigation. The antibody tests used for EBV can not only detect a recent infection, but also a past infection.
EBV is a highly contagious type of herpes virus that is spread through saliva and other bodily fluids. Once you get EBV, it goes dormant and stays in the body forever. It can be reactivated and cause you to get sick again, regardless of how long it’s been since you were first infected.
Testing is appropriate when someone has symptoms of mono or a suspected reactivation of the virus. Testing may also be appropriate when a person has unexplained fatigue.
There is a lot of overlap between EBV, Chronic Fatigue Syndrome, and Long COVID. Testing for EBV can help your provider understand what your recovery path may look like by testing for the larger picture of your health.
What Are the Different Types of EBV Tests?
Antibody tests help determine if someone has been infected with the Epstein-Barr virus and whether the infection is a new infection or a past infection. Blood work can also show the timeline of infection and identify the stage of which it is. Typical antibody tests used to detect EBV include:
- Viral Capsid Antigen (VCA) Immunoglobulin M (IgM) (VCA IgM)
- Viral Capsid Antigen (VCA)-Immunoglobulin G (IgG) (VCA IgG)
- Epstein-Barr Virus Nuclear Antigen (EBNA)
- Early Antigen-Diffuse (EA-D)
Functional medicine practitioners often use a combination of conventional testing and specialized testing to assess EBV activity and its impact on the immune system.
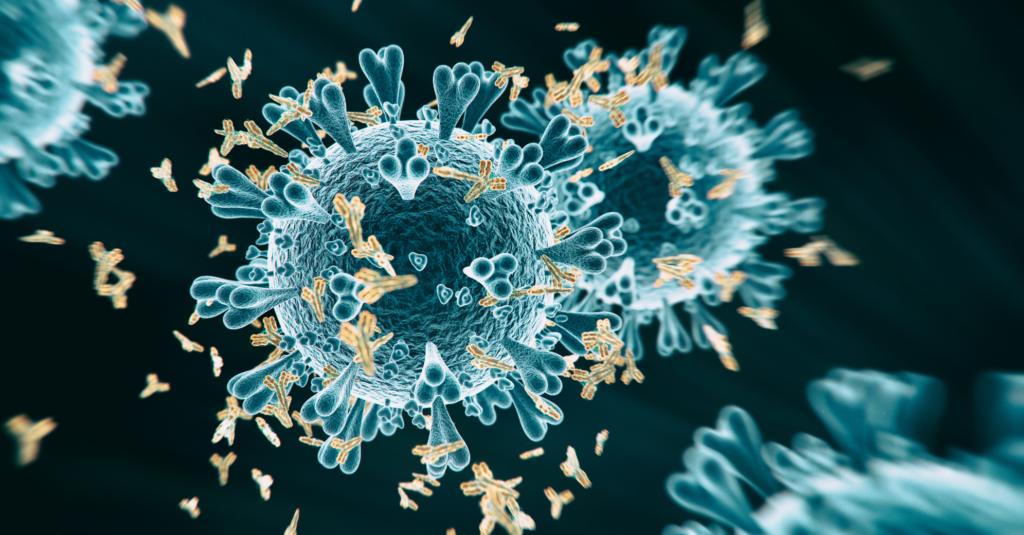
Functional labs analyze antibody profiles and look for certain immune biomarkers to determine the status of EBV infection and potential risks. Such labs help detect patterns of reactivation or immune strain. They also assess the body’s immune response to an EBV infection, including T-cell responses and antibody levels.
Types of functional medicine lab testing may include the following:
- Monospot test, which looks for heterophile antibodies, which are poorly defined antibodies that can interfere with immunoassays, potentially leading to false results
- A PCR (Polymerase Chain Reaction) test detects EBV DNA. It allows for highly sensitive and specific detection and can be used to diagnose infection, monitor viral load, or assess the risk of developing certain EBV-associated diseases.
- EBV antibody tests
- EBV DNA testing, which assesses viral load
- Specialized tests like T-cell immunity tests
Functional lab testing can provide valuable insights into the status of EBV infection and whether or not infection is acute, latent, and cases where immune dysfunction may be affecting the body’s response to the virus.
What Do Each of the Antibodies Mean?
EBV antibody tests help determine if someone has been infected with the Epstein-Barr virus. Test results signal current vs past exposure. A negative test indicates the person has never been infected. A positive test suggests either a current or past infection, with specific antibodies appearing at different stages. Below is a summary of each of the types of tests and what they can indicate:
VCA IgM: Indicates the presence of IgM antibodies against the Viral Capsid Antigen (VCA) of the EBV, a type of virus that can cause infectious mononucleosis (mono). A positive VCA-IgM result usually suggests a recent or current EBV infection, especially if symptoms of mono are present.
VCA IgG: The presence of VCA IgG antibodies indicates a past EBV exposure and is a sign of immunity to the virus. VCA IgG antibodies appear early in the infection and then remain detectable for life.
A positive VCA IgG test without a positive VCA IgM test suggests a previous infection, but the presence of both VCA IgG and IgM indicates an active or recent infection.
EBNA: EBNA antibodies can be detected in blood tests to determine if someone has been infected with EBV.
EA-D: Detects antibodies to the early antigen, indicating a recent infection, reactivation, or chronic infection.
How Can You Tell If EBV Is Reactivated?
After initial infection, EBV goes dormant. It can reactivate at any time, no matter how long it’s been since you were first infected. Factors that cause immune shifts can trigger a reactivation of EBV. These factors often involve a weakened or altered immune response.
Some telltale signs of an EBV reactivation include:
- Extreme fatigue
- Swollen lymph nodes
- Sore throat
- Rash
- Enlarged liver/spleen
Other symptoms that are not well recognized may include:
- Tinnitus
- Malaise
- Brain fog
- Headaches
- Joint pain
- Dizziness
- Anxiety
Antibody levels guide the interpretation of whether or not you may be experiencing an EBV reactivation.
You may have a reactivated infection if you have had a positive EA-D test. However, EA-D alone is not definitive of a reactivation. It must be accompanied by a high VCA IgG and negative EBNA antibodies in an individual with a history of EBV infection may suggest recent EBV reactivation. Here is why:
- EA-D antibodies are usually detected when a person is first infected with EBV and can also show up with a reactivation.
- VCA IgG antibodies are formed during the initial infection and remain positive for life. If you’ve had EBV in the past and a test comes back showing high levels of VCA IgG antibodies, it can indicate a reactivation.
- EBNA antibodies typically appear after the first infection. If you have a negative EBNA result in the presence of positive EA-D and VCA-IgG antibody tests, this might suggest a recent reactivation.
Naturopathic doctors look at the antibody levels combined with symptoms to see if they feel this infection was in the past, or if it’s reactivated. Although the antibodies will be present with a past infection, we look to see how high the antibody levels are. If they are significantly higher than the range, and the patient is presenting with symptoms of EBV, then we would address the case as if it were a reactivation.
How Accurate Is the Monospot Test?
While the Monospot test is a quick and inexpensive test for mono, it has limitations in its accuracy for diagnosing EBV.
The Monospot test is a rapid blood test used to diagnose infectious mononucleosis (mono), which is caused by an EBV infection. Monospot detects heterophile antibodies, which are produced in response to an EBV infection. However, heterophile antibodies are not specific to EBV and can be caused by other viruses.
Monospot doesn’t pick up on EBV-specific information. The test also has a false-negative rate, meaning it may not detect EBV in some cases. False negatives are common early in the illness and also in children.
False-positives may occur when it picks up heterophile antibodies caused by other illnesses.
If Monospot is used, it’s best to also do a follow-up test for an accurate diagnosis. EBV-specific antibody tests (IgM and IgG to viral capsid antigen, early antigen, and nuclear antigen) should be used, especially if the patient is young, and if the Monospot test is negative but symptoms persist.
What’s the Role of Functional or Integrative EBV Testing?
Functional and integrative lab testing play an important role when conventional tests fall short in identifying chronic fatigue or reactivation.
Advanced labs panels complement traditional antibody testing by uncovering systemic patterns of infection, including identifying the stage of infection (acute, latent, or reactivated). These tests go beyond standard serology by helping to pinpoint the specific EBV status and assess the broader impact on the body’s immune system and overall health. They also assist in monitoring disease progression.
Functional lab testing focuses on identifying underlying factors contributing to EBV reactivation or chronic symptoms that go beyond traditional antibody tests, and may include:
- Assessing immune function
- Nutritional deficiencies
- Hormone levels
- Identifying immune markers
- Mitochondrial stress and dysfunction
- inflammation
As a result, an integrative approach to EBV focuses on killing the virus while strengthening the body’s natural ability to heal and may include:
- Immune support
- Nutritional support
- Mitochondrial repair
- Gut health
- Stress resilience
- Sleep management
What Should You Ask Your Doctor When Reviewing EBV Results?
When reviewing EBV test results with your doctor, some key questions you might consider asking include those that focus on understanding your test results and exploring next steps in your approach to managing the infection and its symptoms, such as:
- Do my results indicate a past, recent, or active EBV infection?
- Do my symptoms match the lab results?
- If any results are abnormal, what could be the underlying cause?
- How does my past medical history influence the interpretation of these results?
- Could any of my results indicate a possible link to other health issues or autoimmune conditions?
- What are my treatment options?
- What next steps do you recommend?
- How can I support my body and my immune system in clearing the virus and preventing future reactivations?
- Is it necessary to repeat EBV testing in the future to monitor status?
- Are there any other tests to consider in addition to EBV testing?
- Should there be concern about any long-term effects or complications associated with EBV based on the results?
Test results and symptom tracking help inform approaches to treatment. An integrative approach to care includes an open dialogue between the patient and the provider to help shape care decisions and personalized treatment for better health outcomes.
Questions to ask related to symptom tracking and management include:
- What is the best way to track symptoms, and how frequently should they be recorded?
- Are there any symptoms that are considered a red flag, and when should I contact you?
- Are there specific therapies or lifestyle changes recommended to address particular symptoms?
FAQs
Can EBV tests tell me if I have chronic Epstein-Barr?
EBV tests check for antibodies in the blood and can indicate a current or past infection with EBV, but they don’t definitively diagnose chronic active EBV (CAEBV). CAEBV is a rare, chronic form of EBV infection characterized by persistent symptoms and elevated EBV DNA levels. While EBV antibody tests can help rule out other causes of similar symptoms, they are not the primary diagnostic tool for CAEBV.
What’s the difference between VCA IgG and EBNA?
VCA IgG and EBNA antibodies are both markers for infection with Epstein-Barr Virus, with each indicating a different stage of infection.
VCA IgG can determine the stage of EBV infection – acute, recent, or past. VCA IgG tests are also used to help doctors diagnose infectious mononucleosis (mono).
The presence of EBNA antibodies indicates that a person has had EBV in the past, and the virus is likely dormant in the body.
If my EBNA is positive, am I contagious?
A positive EBNA test means you have been infected with the EBV at some point in your life. It doesn’t necessarily mean you’re contagious. However, it does mean the virus is present in your body and can reactivate and become contagious anytime.
Is there a test for EBV in tissues or organs?
Yes. Tests for detecting EBV in tissues and organs include the following:
- In situ hybridization (ISH), uses probes that bind to specific EBV-encoded RNAs (EBER-1 and EBER-2) to detect their presence in tissue samples. ISH is highly sensitive and specific, making it the preferred method for detecting latent EBV infection.
- Real-time PCR assays can be used to detect and quantify EBV DNA in tissue samples. It is a relatively sensitive test, but it may not be able to pinpoint the location of EBV within the tissue.
- Immunohistochemistry (IHC) is a technique used to detect EBV proteins in tissue samples, helping to identify EBV infection in various organs and tissues, such as tumors. This method is useful for diagnosing EBV-related diseases and understanding the virus’s role in different tissues.
Why are my EBV antibodies still high years later?
EBV is a virus that remains in the body even after the initial infection has subsided. The antibodies produced during that infection lay dormant, but can persist for life. It’s not uncommon for EBV antibodies to remain high or elevated years after an initial infection, but this does not necessarily mean it’s a new infection.
If you are experiencing symptoms, however, the virus may have been reactivated, causing illness again.
Final Thoughts: Interpreting EBV Test Results with Context
Self-diagnosing EBV shouldn’t be done by looking at labs alone. To properly interpret EBV test results, it’s crucial to understand the different antibody tests used and their meaning in the context of EBV infection.
Evaluating the whole person is essential when interpreting EBV test results. Examining lab results alongside an individual’s symptoms provides context and helps inform next steps for the patient.
If you’re curious about your EBV test results, find an integrative practitioner experienced in post-viral and immune conditions who will provide you with personalized and comprehensive care. Such practitioners will evaluate your EBV test patterns and help identify the root cause of your EBV infection. A personalized approach like this leads to clarity and a better informed approach to treatment.
Start your healing journey with us…
- Post Title : How to Test for Epstein-Barr Virus: What Your Results Really Mean
- Author: Dr. Susan Cucchiara, N.D.
- Clinically reviewed by - Dr. Sparks, N.D
- Date Published :